|
Our clinics are closed from 20/12/2025 to 4/1/20206, Merry Christmas and a Happy New Year.
|
Home » Deep Brain Stimulation (DBS) at Melbourne Neurocare
Deep Brain Stimulation (DBS) is an advanced, evidence-based treatment for movement disorders such as tremors and Parkinson’s disease.
DBS is also a potential treatment for a range of neurological and psychiatric conditions, including dystonia, epilepsy, obsessive-compulsive disorder (OCD), and investigational use in Tourette’s syndrome. The potential benefits of DBS include a reduction in symptoms, improved mood, decreased medication requirements, and enhanced quality of life.
At Melbourne Neurocare, our specialists provide comprehensive DBS evaluation, surgical planning, and follow-up care to help patients regain control, reduce symptoms, and improve quality of life.
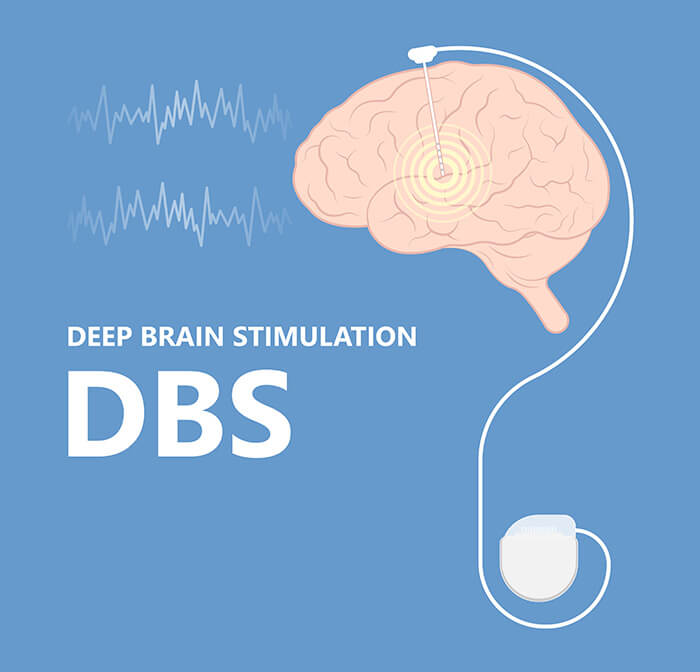
Deep brain stimulation (DBS) is a surgical procedure designed to help people living with movement disorders regain control over their symptoms. By implanting a device that delivers targeted electrical stimulation to specific areas deep within the brain, DBS surgery can significantly reduce debilitating movement symptoms such as tremors, stiffness, and slowed movement. This advanced brain stimulation therapy is most commonly used to treat conditions like Parkinson’s disease, essential tremor, and dystonia, especially when symptoms are not adequately managed by medication alone. The primary goal of deep brain stimulation DBS is to provide consistent symptom control, improve motor function, and enhance the overall quality of life for individuals affected by these challenging neurological conditions.
Deep brain stimulation works by sending carefully controlled electrical impulses to precise brain regions involved in movement control, such as the subthalamic nucleus. These electrical signals help to modulate abnormal brain activity and reduce the problematic electrical signals that cause movement symptoms. The DBS system consists of a pulse generator implanted under the skin of the upper chest, which is connected to thin brain electrodes placed in the targeted deep brain areas. By regulating brain cell activity, DBS therapy can smooth out motor fluctuations and improve motor function, offering relief from symptoms like tremor, rigidity, and involuntary movements. Beyond movement disorders, brain stimulation is also being used to treat conditions such as obsessive-compulsive disorder, Tourette’s syndrome, and chronic pain, highlighting its versatility in managing a range of neurological and psychiatric conditions.
Tremors — involuntary shaking movements — can affect the hands, head, voice, or other parts of the body. Some movement disorders, such as dystonia, can also cause abnormal postures, which may be improved with DBS. They may be caused by conditions such as Essential Tremor, Parkinson’s disease, or other neurological disorders.
For patients whose tremors don’t respond to medication, deep-brain stimulation can be one of the most effective long-term treatment options.
DBS involves a surgical procedure in which DBS electrodes are implanted with precise lead placement into specific brain regions that control movement. These DBS electrodes deliver small electrical pulses to regulate abnormal brain activity, reducing tremors and improving coordination.
Our team works closely with each patient to ensure precise targeting, safe surgery, and optimal programming of the DBS device.
Parkinson’s disease is a progressive neurological condition that affects movement, balance, and muscle control. Deep brain stimulation (DBS) is typically considered for individuals with advanced Parkinson’s disease who experience severe symptoms that are not adequately controlled with medication.
While medication remains the first-line treatment, symptoms such as tremor, stiffness, and slowed movement may become difficult to manage over time. DBS primarily targets motor symptoms such as tremor, stiffness, and slowed movement, but may also have some effect on certain non-motor symptoms.
Deep brain stimulation for Parkinson’s can significantly reduce these symptoms, allowing patients to reduce medication doses and improve daily functioning. DBS can also help reduce medication-induced dyskinesias in Parkinson’s disease, making it a valuable option for those whose involuntary movements are caused by long-term medication use.
For patients with advanced Parkinson’s or severe tremor not controlled by medication, DBS is considered one of the best treatment options available.
In addition to improving movement symptoms, DBS may also help with non-motor symptoms such as urinary urgency.
It is reversible, adjustable, and tailored to each patient — allowing long-term symptom management without destroying brain tissue.
Modern DBS devices have seen remarkable advancements, making the therapy safer and more effective than ever before. A typical DBS device includes a pulse generator, leads, and electrodes. The pulse generator, a small device implanted in the upper chest, produces the electrical impulses that are delivered to the brain. Insulated leads connect the pulse generator to the electrodes, which are surgically implanted in the targeted brain regions. These electrodes deliver precise electrical stimulation to help control symptoms. Today’s DBS devices often feature rechargeable batteries, wireless programming, and customizable stimulation settings, allowing for tailored treatment that adapts to each patient’s needs. These technological improvements mean that DBS therapy can be adjusted over time for optimal results, with minimal disruption to daily life.
Recovery from DBS surgery typically involves a short hospital stay and gradual adjustment of the device over several weeks. A CT scan is typically performed after surgery to confirm accurate lead placement and check for complications such as bleeding. Most patients resume light activities within days, with full recovery taking a few weeks.
Ongoing follow-up ensures the stimulation settings remain effective as symptoms change.
We partner with leading neurosurgeons in Melbourne to perform DBS procedures in state-of-the-art hospital settings. Our role includes:
While DBS is generally safe, potential side effects can include:
These are usually mild and can often be managed by adjusting the device settings.
The cost of DBS varies depending on surgical complexity, hospital fees, and whether you have private health insurance. Medicare and private health funds may cover part of the costs for eligible patients.
Our team provides a clear breakdown of costs before proceeding.
Research shows that DBS can reduce tremors and Parkinson’s symptoms by up to 60–80% in well-selected patients, improving mobility, independence, and quality of life.
Like a heart pacemaker, which is a small device implanted under the collarbone or in the abdomen to deliver electrical stimulation and regulate abnormal heart rhythms, the DBS device is also implanted and delivers electrical stimulation to regulate abnormal brain activity.
Its effectiveness often lasts for many years, with settings adjustable as symptoms change.
Clinical trials and ongoing research have been instrumental in establishing DBS therapy as a leading treatment for movement disorders. Numerous studies have confirmed the effectiveness and safety of DBS in managing conditions such as Parkinson’s disease, essential tremor, and dystonia. Researchers continue to explore new frontiers for DBS, including its potential to treat memory deficits, substance abuse, and other brain conditions. Advances in DBS devices and technology are also being tested, with clinical trials focusing on more targeted stimulation of specific brain regions and the development of next-generation implantable devices. This commitment to research ensures that DBS therapy remains at the forefront of clinical practice, offering hope and improved outcomes for people with a wide range of neurological challenges.
After DBS surgery, ongoing follow-up is essential to ensure the therapy remains effective and safe. Regular appointments allow your care team to monitor your progress, adjust stimulation settings, and address any concerns. The pulse generator’s battery life typically lasts several years, depending on the type of device, and replacing the battery is a straightforward procedure compared to the initial implantation. Many patients experience a reduction in their medication needs after starting DBS therapy, so it’s important to keep track of any medication reduction and discuss changes with your doctor. While DBS is generally well-tolerated, it’s important to report any new symptoms, such as infection, bleeding, or signs of cognitive decline, to your healthcare provider promptly. With proper follow-up and maintenance, DBS therapy can provide long-term relief from debilitating movement symptoms and help individuals with movement disorders maintain a better quality of life.
You may be a candidate if you have Parkinson’s or tremor symptoms not adequately controlled by medication, are in good general health, and have no severe cognitive impairment.
No — DBS does not stop disease progression but can greatly reduce symptoms and improve daily function.
Batteries typically last 3–5 years for non-rechargeable systems, and up to 15 years for rechargeable ones.
While DBS can influence mood or thinking in some cases, most patients do not experience significant personality changes. Adjustments can be made if side effects occur.
Age alone is not a disqualifying factor; overall health and suitability are more important considerations.
If tremors or Parkinson’s symptoms are affecting your independence, deep brain stimulation may be an effective solution.
📞 Call 1300 080 784 or Book Online to discuss your suitability for DBS with our specialist team.